Breast cancer. The words alone terrify most women, and a diagnosis can be shattering. But there’s a growing reason for optimism. The disease is being detected at earlier, more curable stages, and there’s an increasing variety of treatment options.
Breast cancer is the most common type of cancer among American women. Experts estimate that of the women who live to be 85, one in nine will get the disease at some point in her life. In fact, each year, more than 175,000 women are diagnosed with breast cancer–that’s equivalent to a woman learning she has it every three minutes. An estimated 46,000 women died of the disease in 1994 alone. Only lung cancer causes more cancer deaths among women.
The greatest risk factor for developing breast cancer is being female. A prior history of the disease increases the risk as well. Here are some other factors associated with an increased risk.
- Age. About 75 percent of all breast cancers are found in women over the age of 50. The disease is uncommon in women under the age of 35 and quite rare in women under the age of 25 (see chart).
- Family History. Risk increases if a woman has a mother or sister who has had breast cancer before menopause.
- Early Menstruation. A woman whose first menstrual period was before the age of 12 is at higher risk.
- Late Menopause. Having started menopause after the age of 55.
- Delayed Childbearing. Never having had a child or having the first child after the age of 30.
- Diet. A diet high in fat has long been thought to increase the risk of breast cancer, but a recent Harvard study disputes that belief. Researchers there reviewed studies involving nearly 338,000 women and found that even extremely low fat diets (less than 20 percent of calories from fat) failed to reduce breast cancer risk.
- Smoking. Recently, an ACS study found that while smoking may not cause breast cancer, it does seem to increase a woman’s chance of dying from the disease by 25 percent.
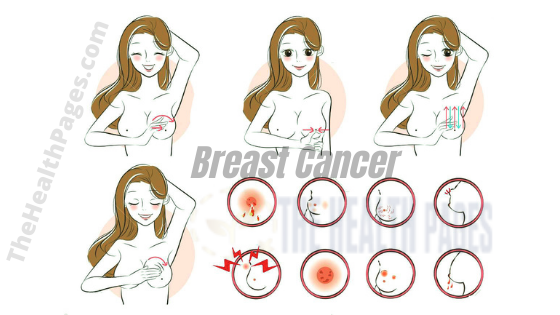
You should see your doctor if you notice any of the following changes in your breasts:
- A lump in the breast or under the arm.
- A change in the normal size or shape of your breast.
- Spontaneous discharge coming out of your nipple.
- A change in the color or feel of the skin of the breast or areola.
- A sudden onset of pain in the breast.

What Is The Best Defense Against Breast Cancer?
Early detection .To ensure the widest range of treatment options, it is important to detect breast cancer as early as possible. With prompt treatment, the outlook for cure is good. According to the National Cancer Institute (NCI), the five-year survival rate for women whose tumors haven’t spread beyond the breast is 92 percent. When the cancer has spread to nearby lymph nodes under the arm, the rate decreases to 71 percent, dropping drastically to 18 percent once the cancer has spread to the liver, lungs or brain.
There are three main ways women should screen for breast cancer:
1) Breast Self-Examination. Women’s breasts come in many sizes and shapes. Age, menstruation, pregnancy, menopause and taking birth control pills or other hormones can all cause breast changes. It is important to learn what is normal for you. This can be done by regularly examining your breasts. A breast self-examination (BSE) is easy to do and a good way to take charge of your health.
Beginning at age 25, women should do a BSE regularly after menses. Being familiar with the usual appearance and feel of your breasts will make it easier to notice any changes from month to month. If you discover any of the symptoms listed above, see your doctor as soon as possible.
Click here to see how to perform BSE.
2) Physical Breast Exam. Periodic breast examination, or palpation, by a health professional is an important step in early detection. During the exam, the doctor feels the breast and underarm with his or her fingers, checking for lumps. All women should have breast examinations as part of their routine checkups. Women 30 and older should have them annually.
3) Mammography. A mammogram is an x-ray of the breast. It can reveal tumors and other changes in the breast too small to be felt by hand. When high-quality equipment is used and the x-rays are read by well-trained radiologists, 85 to 90 percent of cancers are detectable. Of the 10 to 15 percent of cases that don’t show up on mammograms, most occur in younger women since they have denser, more fibrous breast tissue.
How a mammogram works: The breast is placed between two plates and pressure is applied to ensure a clear picture. That pressure may be uncomfortable, but the test only lasts a few minutes. Two x-rays are taken of each breast, one from the top and one from the side. Although some women are concerned about the risk of cancer posed by radiation during mammography, the actual risk is very small.
There has been a lot of debate over the past few years about whether women between the ages of 40 and 50 should have regular mammograms. The National Cancer Institute (NCI) had withdrawn this general recommendation, saying there was no conclusive evidence that regular mammograms reduce the death rate from breast cancer of women under 50. However, in March, 1997, it announced that it once again supported mammography screening in this age group. Other organizations, including the American Cancer Society and the American Medical Association, have always recommend women have routine mammograms every one or two years after age 40 and annually after age 50.
How Is Breast Cancer Diagnosed?
A biopsy is the only sure way to know whether a breast lump or a suspicious area seen on a mammogram is, in fact, cancer. A biopsy is a microscopic analysis of cells taken from the lump to determine if they are cancerous. The cells can be obtained by fine-needle aspiration, in which a few cells are extracted using a thin needle and a syringe, or open biopsy, in which a larger sample of tissue is surgically removed.
The good news: Four out of five breast lumps are not cancerous. Often the lump is a fluid-filled cyst, which can be drained through needle aspiration or diagnosed by ultra-sound. If the lump is a solid tumor, a biopsy should be performed for tissue analysis. Frequently, the lump is removed at the time of biopsy. If the lump is left in place, a tissue diagnosis should be obtained by fine-needle aspiration or core needle biopsy, in which a larger tissue sample is drawn out. The lump should then be checked regularly for changes.
What Are The Treatment Options?
The choice of treatment for breast cancer depends on the stage of the cancer (whether it has spread to other places), the type of breast cancer, and certain characteristics of the cancer cells (such as how fast they are growing). The woman’s age, whether she has had menopause and her general health, also help the doctor develop a treatment plan that best fits the woman’s individual circumstances and values.
A woman might want a second doctor to review her diagnosis and treatment plan. A short delay in beginning treatment should not reduce the chances of its success.
The treatment options for breast cancer are surgery, radiation therapy, chemotherapy and hormone therapy. The doctor may recommend just one method or a combination, depending on the patient’s needs. In some cases, a woman may be referred to other doctors for different therapies, such as oncologists for chemotherapy.
1) Surgery. There are several different types of surgery for breast cancer. Here are some of the options:
- Breast conserving surgery (lumpectomy, partial mastectomy, quadrantectomy) removes just the cancerous lump with some surrounding healthy breast tissue and usually some lymph nodes from under the arm. About two to three weeks after surgery, patients begin radiation therapy, which generally consists of a five-day-a-week regimen for six weeks. Research has shown that when combined with radiation, lumpectomy is as effective as mastectomy in treating early stage breast cancer and is preferable since a women retains her breast.
- Modified radical mastectomy removes the breast, the lymph nodes under the arm and the lining over the chest muscles (leaving the muscles intact). This procedure is an alternative to breast conserving surgery and radiation therapy. Due to long held beliefs by physicians and patients, this remains the most common type of surgery for breast cancer.
- Total or simple mastectomy removes the breast and the lining over the chest muscle below the tumor. It is used to treat extensive ductal carcinoma in situ (abnormal cells found in the milk duct). It is also done to prevent breast cancer in women at inordinately high risk of developing the disease due to a defective gene, which may account for about five percent of all breast cancers.
Click here to see how much of your breast each type of surgery removes.
2) Adjuvant Therapy. A doctor may advise a woman with early stage breast cancer to supplement surgery with another form of therapy. Called adjuvant therapy, this added regimen can help prevent cancer from recurring by killing cancer cells that may still be lingering in the body undetected.
- Radiation Therapy (or radiotherapy) uses high-powered rays to damage cancer cells and stop them from growing. Radiation may come from an x-ray machine outside the body (external radiation) or from radioactive materials placed directly in the breast through thin plastic tubes (implant radiation). Sometimes both are used.
- Chemotherapy uses drugs to kill cancer cells. These drugs may be taken orally or injected into a muscle or vein. Chemotherapy is administered in cycles-a treatment period followed by a rest period, then more treatments, and so on. Although it depends on the type of drugs used, chemotherapy generally does not require a hospital stay.
- Hormone Therapy keeps cancer cells from getting the hormones they need to grow. If tests show the cancer is receptive to hormones, drugs may be administered to alter the way the hormones work or surgery may be performed to remove organs (such as the ovaries) that manufacture the offending hormones.
What Can I Do to Protect Myself?
You can take charge of your health care by examining your breasts regularly and deciding, in consultation with your doctor, what screening course is best for you-and then sticking to it. Moreover, tell the women in your life, your mother, your sister, your daughter, to do the same.
Our thanks to Mary Jane Houlihan, M.D., Beth Israel Hospital, Breast Care Center, Harvard Medical School, Boston, MA, for reviewing this article.
| By Age: | Risk Equals: |
| 25 | 1 in 19,608 |
| 35 | 1 in 622 |
| 45 | 1 in 93 |
| 55 | 1 in 33 |
| 65 | 1 in 17 |
| 75 | 1 in 11 |
| 85 | 1 in 9 |
| Over 85 | 1 in 8 |
How Screening can save your life
Average size of lumps found…
Source: Breast Health Program of New York
While mammograms are tops for finding the tiniest lumps, they aren’t full-proof. That’s where life- and breast-saving lies in your hands. Your self-exam could detect lumps small enough to be removed by lumpectomy.
Breast self-examination should be done on a regular basis so you can become familiar with the usual appearance and feel of your breasts. If you menstruate, the best time to do BSE is 2 or 3 days after your period, when your breasts are least likely to be tender or swollen. As you become more comfortable with the procedure, you may want to experiment with other methods to see what works better for you. You can also ask your doctor to show you how to do BSE.
| 1) Stand before a mirror. Inspect both breasts for anything unusual such as discharge from the nipples or puckering, dimpling, or scaling of the skin. |  |
The next two steps are designed to emphasize any change in the shape or contour of your breasts. Feel for any unusual lump or mass under the skin. As you do them, you should be able to feel your chest muscles tighten.
| 2) Watching closely in the mirror, clasp your hands behind your head and press your hands forward. |  |
| 3) Next, press your hands firmly on your hips and bow slightly toward your mirror as you pull your shoulders and elbows forward. |  |
Some women do the next part of the exam in the shower because fingers glide over soapy skin, making it easy to concentrate on the texture.
| 4) Raise your left arm. Use your right hand to check your left breast thoroughly. Beginning at the outer edge, press the flat of your fingers in small circles, moving around the breast, working toward the nipple. Explore the area between the breast and the underarm as well. |  |
| 5) Look for any spontaneous discharge from the nipple. Repeat steps 4 and 5 on your right breast. |  |
| 6) Repeat steps 4 & 5 lying down and using the same circular motion. Lie flat on your back with your left arm over your head and a pillow or folded towel under your left shoulder. This position flattens the breast and makes it easier to examine. |  |
Repeat the exam on your right breast.
Source: National Cancer Institute
Women in their 40s are confused about whether or not to get yearly mammograms. And for good reason. For the past several years, experts have been batting different recommendations for this age group back and forth. The debate heated up again in early 1997 when an expert panel of the National Institutes of Health (NIH) said there was no evidence that mammograms save the lives of women under 50. Yet a few months after that pronouncement, the National Cancer Institute (NCI), which is affiliated with the NIH, said women in their 40s should have breast x-rays every one to two years. Why is this issue so hotly contested, and what are the latest recommendations?
There’s no doubt that annual mammograms for women aged 50 and older save lives. Many studies show that for these women the decrease in mortality rate is as high as 30 percent. But for younger women, several factors muddle the mammogram picture:
- Women in their forties have lower rates of breast cancer than do older women. Of 1,000 women in their forties, 16 will get breast cancer, compared with 25 out of 1,000 in the next decade of life. Scientific evidence does not show that mammograms would save these 16 lives.
- Younger women have denser breast tissue, making mammograms harder to interpret accurately. A small number of dangerous cancers (25%) in this age group will be missed by the x-ray exams.
- The younger the woman the greater the risk of getting a false positive result (detecting something that is not cancer) from a mammogram. Such results can create anxiety and may lead to unnecessary biopsies or surgeries.
Despite all this, the following arguments are made in favor of regular mammograms for fortysomething women:
- Women who get mammograms regularly are more likely to get other necessary medical care, such as Pap tests and professional manual breast exams (palpation).
- Cancer in younger women usually grows faster, making early detection all the more important.
- Certain studies show that mammograms for younger women can decrease cancer deaths. But some say this evidence is weak since the advantage does not become clear until these women are in their fifties.
The American Cancer Society (ACS) currently recommends that women in their forties at average risk for breast cancer get a mammogram every year. The NCI recommends screening every one to two years.
| Lumpectomy removes just the breast lump and usually the lymph nodes under the arm. |  |
 | Modified Radical Mastectomy removes the breast, the lymph nodes under the arm and the lining over the chest muscles (leaving muscles intact). |
| Partial or Segmental Mastectomy removes the tumor, some of the normal breast tissue around it, and some lymph nodes. |  |
 | Total or Simple Mastectomy removes the tumor, some breast tissue around it and the lining of the muscle below the tumor. |
Cancer Information Service
A National Cancer Institute telephone service set up to answer questions from the public nationwide.
800-4-CANCER
American Cancer Society (ACS)
The group’s “Reach to Recovery” trains volunteers, who have had breast cancer themselves, to visit patients and provide emotional support before and after treatment.
800-227-2345
Y-Me
A toll-free hotline staffed by women with breast cancer. In addition to providing information, Y-ME can direct callers who want to volunteer time or money to a breast cancer organization.
800-221-2141